“The olfactory sense is the only sense that has direct access to the memory centers of the brain and [aromatherapy] is a good way to stimulate those centers with little effort.” –Dr. Michael Leon, professor emeritus of neurobiology and behavior at the University of California Irvine.
June is National Alzheimer’s and Brain Awareness Month. Fleur’s comfort care products help you take care of your brain.
As a Flower Essence Aromatherapy practitioner and the daughter of a mother with Alzheimer’s, I’m committed to raising awareness about dementia, a condition that affects millions of lives worldwide.
Whatever your age, now is the right time to take actions that help promote a healthy brain. Get familiar with brain health and learn what steps you can take if you or someone you love has memory concerns.
In this blog post, I’ll provide an overview of what happens to the brain with Alzheimer’s disease and how it impacts memory.
Furthermore, I will provide valuable insights on how aromatherapy can slow cognitive decline, making it worthwhile. I will highlight several essential oils that enhance working memory and improve brain function.
Lastly, I will discuss the benefits of Fleur Clarity & Focus Spray in relieving symptoms associated with memory disturbances in individuals experiencing brain degeneration and other forms of dementia.
Dementia Diversity
Dementia is not a specific disease. It’s an umbrella term to describe a range of neurological conditions affecting the brain that worsen over time. These conditions include problems with memory, thinking, or language and changes in mood, emotions, perception, and behavior.
Dementia is a general term for loss of memory and other mental abilities severe enough to interfere with daily life—physical changes in the brain cause it.
Various forms of dementia affect individuals in unique ways. The speed at which dementia progresses differs greatly from person to person. Some individuals may live well with dementia for an extended period, while others may experience a rapid decline.
Alzheimer’s is the most common type of dementia, but there are many kinds. Memory loss, a common sign of Alzheimer’s disease, often involves forgetting recently learned information, especially in the early stages.
Others include forgetting important dates or events, asking the same questions repeatedly, and increasingly needing to rely on memory aids (e.g., reminder notes or electronic devices) or family members for things they used to handle on their own.
For a loved one with dementia, life can be frustrating, confusing, and scary. Cognitive decline refers to changes in thinking ability that occur as people age.
Some changes are to be expected, but there are concrete steps you can take to mitigate their impact and slow down the decline.
Alzheimer’s and Dementia
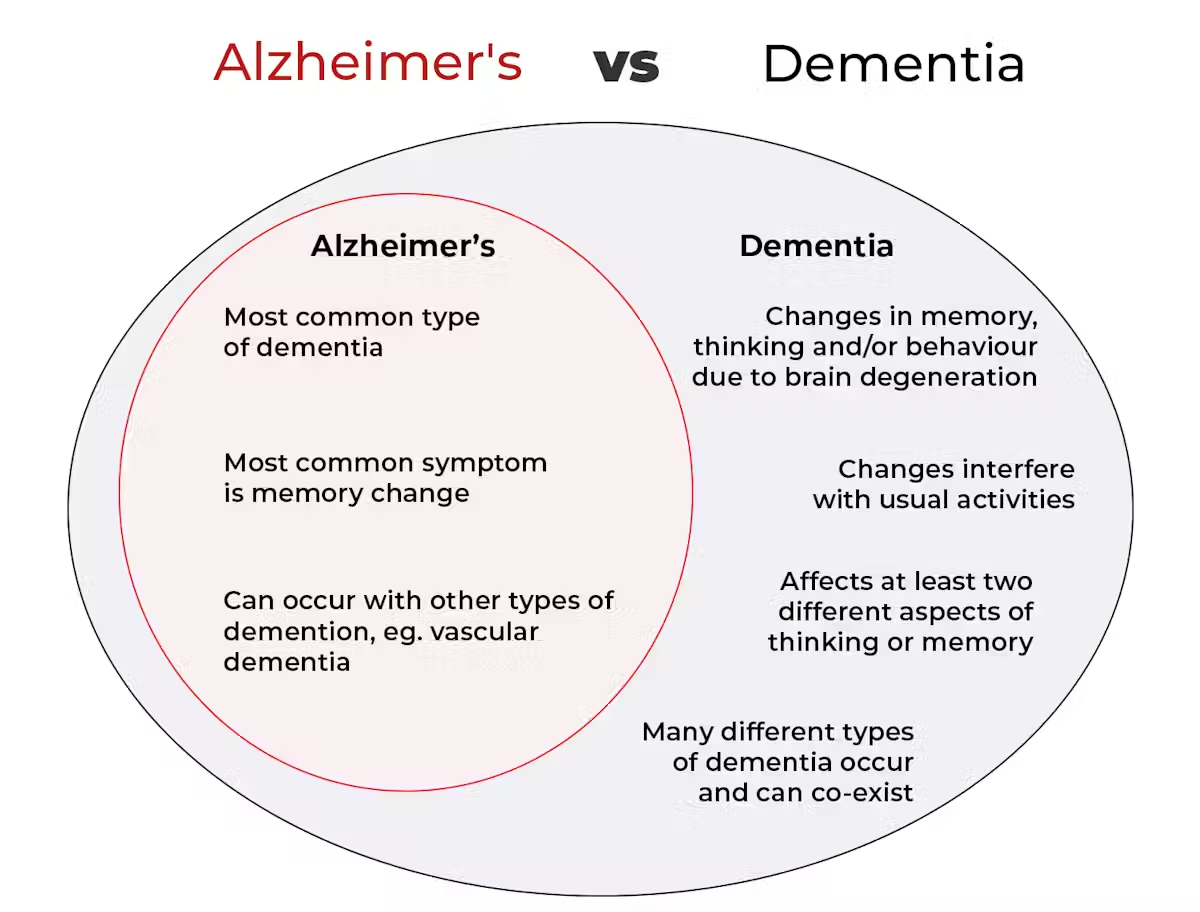
Worldwide, 55 million people are living with Alzheimer’s and other dementias. Alzheimer’s is a degenerative brain disease that causes a slow decline in memory, thinking, and reasoning skills.
- Dementia is a term for various brain disorders that affect memory, thinking, behavior, and emotion.
- Dementia knows no social, economic, or ethnic boundaries.
- Dementia is the leading cause of disability and dependency among the elderly.
- Each person experiences dementia in their own way, but generally, those affected eventually need help with all aspects of daily life.
- There is currently no cure for dementia, but we can reduce its advancement through lifestyle and aromatherapy strategies.
Early symptoms of dementia can include
- memory loss
- difficulty performing familiar tasks
- problems with language
- personality changes.
In Alzheimer’s patients, agitation is a common issue. Unfortunately, dementia medications often have limited effectiveness, especially in addressing cognitive decline or distressed behaviors.
Understanding Brain Changes
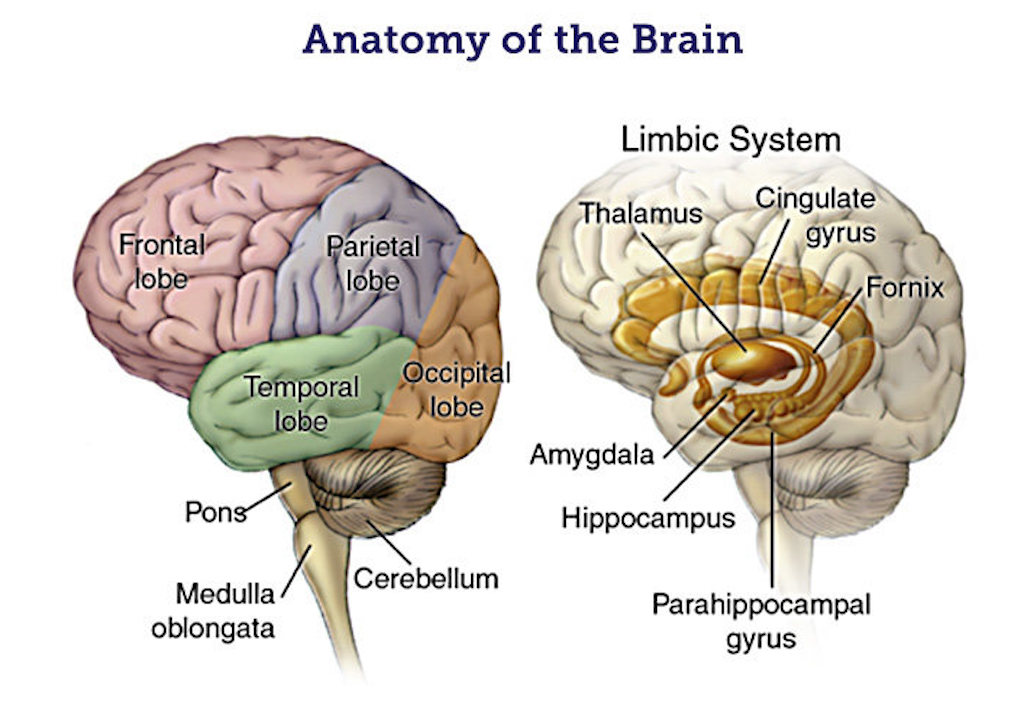
Knowing more about the brain and how it changes can help us understand the symptoms of dementia. It can also help or support a person with dementia in living well.
Reviewing the brain’s functions helps understand vision, language, and behavior difficulties. Depending on the damaged parts of the brain, a person with dementia will experience symptoms impacting all aspects of functional and relational living.
 The Cerebral Cortex
The Cerebral Cortex
The cerebral cortex is a thin layer of cells covering the outside surface of the brain. It is responsible for:
- memory
- reasoning
- decision-making
- language
- social skills.
It controls actions such as movement and communication and processes sensory information, including sight, hearing, taste, smell, touch, and pain.
100 billion Nerve Cells – 100 Trillion Synapses
The brain’s essential activity takes place inside individual cells. Cellular activity patterns demonstrate how our brains encode our thoughts, memories, skills, and sense of identity at the cellular level. Over time, our experiences create patterns in signal type and strength.
Alzheimer’s disease destroys neurons, the primary brain cells. It disrupts electrical conduction and neurotransmitter function, leading to cell death and tissue loss. Therefore, the brain experiences significant shrinkage, which impacts all functions.
The function and survival of neurons depend on several key biological processes:
- Neuronal communication through networks of cells generates an electrical charge that travels down the length of its axon and releases neurotransmitter chemicals across a tiny gap called a synapse. The early loss of synaptic connections is one of the main hallmarks of cognitive decline associated with Alzheimer’s.
- Metabolism involves the breakdown of chemicals and nutrients within a cell, which is crucial for healthy cell function and survival. In individuals with Alzheimer’s disease, glucose enters the brain less frequently, and energy production is reduced, which impacts neurons due to their high energy requirements.
- Repair, Remodeling, and Regeneration. Unlike many cells in the body, which are relatively short-lived, neurons have evolved to survive a long time, and some keep working throughout a person’s lifetime. In people with Alzheimer’s, there is evidence suggesting the areas of the brain involved in memory and learning.
Brain Damage & Functioning
Alzheimer’s disease is a devastating disease. It damages more areas and lobes of the brain, leading to a thinning of the cortex, loss of older memories, and gradual brain shrinkage.
Damage to the left hemisphere is linked to problems with semantic memory and language, so someone may struggle to find the right word for something.
Injury to the temporal lobes can make it difficult to recognize familiar faces and objects. People with Alzheimer’s disease may respond to someone on an emotional level, even if they do not recognize them.
Interestingly, even though people with Alzheimer’s may struggle with visual recognition, they may still be able to identify a person once they hear them speak, as the pathways for vision and hearing are separate.
If the right parietal lobe is damaged, the person might have problems judging distances in three dimensions. Navigating stairs is a common difficulty.
As the damage spreads to the frontal lobes, someone with Alzheimer’s may struggle with decision-making, planning, or organizing (e.g., family finances). A more complex task with a sequence of steps, such as following a new recipe, might also become much more challenging.
In contrast to these losses, many abilities are retained, particularly those acquired long ago. Learned skills such as dancing or piano play rely on procedural memories, primarily stored deep within the brain. In Alzheimer’s disease, these skills are often retained the longest.
The Limbic System’s Role in Memory
The limbic system is a collection of regions in the brain that are involved in processing emotions. It includes the
- amygdala
- hippocampus
- hypothalamus
- thalamus.
Damage to the limbic system is typical in most forms of dementia. In Alzheimer’s disease, the hippocampus and its connected structures are often the first to be damaged. As a result, it becomes much harder for someone to form new memories or learn new information.
The hippocampus is vital for recalling memories but less critical for retrieving older memories. Damage to the hippocampus in early-stage Alzheimer’s can lead to difficulty remembering recent events, causing repetitive conversation.
In Alzheimer’s disease, the amygdala is affected later than the hippocampus. This means that a person with Alzheimer’s may remember the emotional aspects of something even if they don’t recall the factual details. As a result, they may respond more based on their feelings rather than logically.
Sensory Changes with Dementia
We take for granted that what we see, hear, smell, taste, and touch is concrete reality. One often overlooked consequence of dementia is its effect on the body’s five senses.
If you are caring for a loved one with dementia, sensory changes are essential to be aware of to keep your loved one safe and engaged.
Sight
However, for people with dementia, the connection between sight and the brain’s ability to interpret some images could be impaired. This can cause confusion, anxiety, and issues in identifying familiar faces, places, and objects.
Seeing colors and shapes may not make sense, even causing them to fear walking or navigating steps because they may interpret flooring transitions as dangerous.
Hearing
Dementia, particularly Alzheimer’s, can affect hearing. The disease causes difficulty processing certain sounds and words. When someone has difficulty hearing, in addition to the effects of dementia, this can commonly cause confusion and anxiety.
Keeping a calm and quiet environment with little background noise is optimal for eliminating confusion and anxiety. Playing soft music, particularly those from their younger years, helps the brain remain active and brings a sense of familiarity to their lives.
Taste
Taste and smell are intricately woven and change significantly with dementia. Many people with dementia experience sudden changes in eating habits and crave unhealthy foods rich in sugar.
Mouth nerves in the mouth are connected to the brain, and when these nerves are affected, the brain can experience a bad taste associated with them.
Taste buds also diminish as dementia and Alzheimer’s progress. People with dementia do not taste food or experience flavor like they once did, leading to appetite changes. Also, chewing is impaired.
Another challenge may be feeling overwhelmed by food choices or forgetting to eat and drink. Caregivers must monitor the diets of dementia patients to ensure proper nutrition and hydration, which is critical to maintaining their health.
Touch
Lastly, I wanted to mention the importance of gentle touch for a person with dementia. Human contact through touch is a critical way to convey connection and care.
Touch can play an essential role in the wellbeing of people with dementia. It can help with a range of conditions associated with dementia, such as anxiety, depression, and agitated behavior. Touch can also help communicate and form bonds, especially for nonverbal people.
 Touching your loved one by hugging, holding hands, applying lotion, or giving a gentle massage is critical to their wellbeing.
Touching your loved one by hugging, holding hands, applying lotion, or giving a gentle massage is critical to their wellbeing.
Understanding how dementia affects the senses can make you a better caregiver and help you prepare for the changes experienced by a loved one with dementia.
Awareness of and recognizing changes in your loved one’s senses allows you to take precautions and avoid unnecessary confusion, anxiety, and dangerous situations to ensure their safety.
Olfactory Impairment
Like taste, olfaction plays a crucial role in various brain processes, particularly the emotional processing of stimuli.
Olfactory impairment, cognitive function, and behavioral and psychological symptoms in various neurological disorders are known to be interrelated. Smells, memories, and emotions are often closely intertwined, as scent-triggering recollections tend to be deeply rooted in our earliest memories.
Olfactory impairment occurs in all patients with Alzheimer’s disease (AD), 90% of patients with Parkinson’s disease (PD), 98% of patients with frontotemporal dementia, and 15% of patients with vascular dementia.
Working Memory
Working memory describes the brain’s ability to hold and process information. Crucial for various cognitive functions, working memory involves the mechanisms that form, retain, and recall memories, allowing us to perform a task without relearning it.
Cognitive loss in older adults is a growing issue in our society, and there is a need to develop inexpensive, simple, effective in-home treatments.
Aromatherapy can improve working memory by engaging the senses and stimulating the brain’s olfactory bulb and limbic system.
The Proust Effect
The connection between aromatherapy and cognition is firmly rooted in science. Our olfactory system, responsible for our sense of smell, triggers emotions and memory.
What makes smells so unique?
The exceptional ability that smells have to trigger memories is known as “the Proust effect” due to how close the olfactory processing system is to the memory hub in the brain. Its effect relates to how memories are processed and how smells stimulate retrieval.
While other stimuli can also (obviously) make us recall memories, they are usually not as detailed, sudden, or vivid as those related to smells. Certain smells can suddenly and involuntarily transport us to a specific time and place.
A new study published in Nature Communications shows that our brains integrate smell with information about space and time to form episodic memories. Odors can instantly trigger vivid autobiographical memories.
For example, the Proust phenomenon can manifest in various ways, such as the pleasant aroma of cookies evoking childhood memories or, more hauntingly, triggering PTSD recollections.
Thus, individuals experiencing cognitive decline may benefit from increased odor stimulation, which can enhance the brain’s memory centers and overall memory function.
My Mother
Before my mother was diagnosed with Alzheimer’s, she was an independent woman who loved to socialize and travel. She was fastidious and loved order and beauty in her living environment. Sadly, her life took a turn when she started showing symptoms of dementia.
 Her memory symptoms came on gradually, but she kept what she was experiencing from her family. She was a woman who cared about others’ opinions and felt embarrassed when she forgot necessary appointments, misplaced her wallet, or got lost.
Her memory symptoms came on gradually, but she kept what she was experiencing from her family. She was a woman who cared about others’ opinions and felt embarrassed when she forgot necessary appointments, misplaced her wallet, or got lost.
She frequently put things in unusual places, unable to go back over her steps to find them again, which frightened her. As a result, not only did her cognitive abilities suffer, but as a woman living by herself, she became increasingly aware of her memory challenges and felt a great deal of shame.
My mother was a fiercely private person and had successfully looked after her finances. However, dealing with financial and legal matters was alarmingly overwhelming and confusing for her as her disease progressed.
Unfortunately, she became a victim of elder financial exploitation. Sadly, when we intervened, this situation caused my mother to feel anger and resentment. Initially, she withdrew emotionally from us and blamed us for what she perceived as attempts to control her.
Impacted Relationships
Relationships are complex at the best of times. Add to these are the dilemmas faced by partners and families affected by Alzheimer’s disease.
Watching a friend or family member suffer from a neurodegenerative disease, such as Alzheimer’s or dementia, creates powerful feelings of helplessness, grief, frustration, and even anger.
As my mother became more socially isolated, she also became emotionally angry and combative. Due to her increased stress, anxiety, and fear, she particularly struggled during interactions with other people, especially groups of people. Following a conversation was difficult at best, thus the repeated questions.
My sisters and I found ourselves in new roles with our mother. Because my mother could not handle her basic needs, such as personal hygiene and household chores, caring for her also caused significant stress for our family.
Finally, to ensure her safety, we helped her to move into assisted living. Throughout my mother’s decline, we recognized that necessary changes in a familiar environment with known objects and routines created significant stress. The introduction of new or unfamiliar people profoundly impacted her mood and heightened her anxiety.
I am deeply thankful to my sisters for their compassionate and diligent management of our mother’s transition and personal affairs. Their dedication ensured that she received the care she deserved.
Rate of Progression
The rate of progression varies greatly. On average, a person with Alzheimer’s lives four to eight years after diagnosis but can live as long as 20 years, depending on other factors. The course of the disease depends in part on age at diagnosis and whether a person has other health conditions.
My mother’s gradual decline down the slippery slope of Alzheimer’s disease took many years. At the age of 71, in September 2002, she first expressed anxiety about her forgetfulness. I suspect her memory had been failing for many months (perhaps years) before.
She was formally diagnosed in 2003, which was a critical period of decision-making for the family to determine where she would live and who would care for her.
During that period, we were unaware of the multifaceted manifestations of her progressive neurological condition and its underlying pathology.
 In 2005, soon after we relocated her back to California so that my younger sister and her family could be near, her decline took a new turn. But she was still living on her own.
In 2005, soon after we relocated her back to California so that my younger sister and her family could be near, her decline took a new turn. But she was still living on her own.
Over the next five years, her condition steadily worsened. By 2010, she was a mere shadow of her former self, barely able to engage with us. Her memory had faded, and she struggled to communicate her thoughts. It was no longer safe for her to live without daily care.
We began liquidating her remaining assets and moved her to a small assisted-care home setting with wholesome meals. She seemed to stabilize in this environment for a couple of years.
Sadly, the facility closed, and we had no choice but to move her to a Medi-Cal dementia care facility when that happened.
Through this period, my mother no longer recognized me as her daughter. I didn’t take her inability personally but felt immense compassion and cherished our moments together.
Kindness & Care
Over the subsequent years, during my monthly visits, I made a point of simply being with her, using kindness and care to connect with her humanity and, most importantly, her spirit.
I maintained a gentle speaking tone and made meaningful eye contact with her. I would mist her with Anxiety Relief Spray and alternate with Amore Love Spray. She instinctively would take deeper breaths, smile, and say, “That’s nice.” Her eyes would start to sparkle, and she would become more alert, although she could not name what she was smelling.
I applied Praśānta Calming Body Oil (lavender and sweet orange) and gently massaged her dehydrated hands and forearms, creating a relaxing and connecting experience for us. She would smile and say, “That’s nice. You’re good and loving.”
These are a few of my precious memories with my mother before she passed away in 2016.
Boost Cognitive Function with Botanical Essential Oils
Aromatherapy does not target the root cause of these illnesses. What it can do, however, is ease the symptoms brought on by Alzheimer’s and dementia.
Aromatherapy’s remarkable benefit in memory care is its ability to enhance cognitive function. The sense of scent, combined with the sense of touch, will reach the person’s innermost parts through the fog of Alzheimer’s disease.
Our senses can worsen as a result of disease and old age. However, while impairment to hearing or vision is quickly apparent, a decline in our sense of smell can be insidious, with months or even years passing before it becomes obvious.
Olfaction, or the sensation of smell, is considered the most evolutionarily ancient sense, as evidenced by the direct anatomical connections between the olfactory cortex and the limbic system.
New research shows that olfactory stimulation is crucial in the symptoms and severity of neurodegenerative diseases in older individuals. Smelling certain essential oils sends positive signals to the limbic system via the central nervous system, where they can influence mood, feelings, and cognitive function.
Moreover, frequent exposure to various scents also referred to as olfactory enrichment, has been shown to have the potential to improve cognitive abilities in older adults.
Agitation and anger due to memory loss and confusion are significant symptoms of dementia and Alzheimer’s. Several essential oils, like lavender, bergamot, and lemon, are proven to calm symptoms and help to soothe agitation.
The direct impact of essential oils through the olfactory system frequently elicits a positive emotional response, which can reduce significant clinical agitation in patients with Alzheimer’s disease.
Key Essential Oils for Cognitive Enhancement in Dementia
Essential oils have been found to directly enhance brain function, especially in the frontal lobe and limbic areas of patients with dementia.
Patients with Alzheimer’s can experience improvements in cognition, emotions, and physical well-being through the use of essential oils in aromatherapy, leading to enhanced quality of life and reduced symptoms.
Aromatherapy can effectively address the difficulties of Alzheimer’s dementia by utilizing essential oils to enhance mental, emotional, and physical well-being.
Some studies suggest that regular exposure to various scents, known as olfactory enrichment, can positively affect cognitive abilities in older adults. Essential oils such as rosemary and peppermint have been proven to enhance memory recall, improve concentration, and stimulate the mind.
Smells can trigger long-forgotten memories, and several studies show that aromatherapy produces significant cognitive improvement in seniors who struggle with these diseases. While it may not cure your loved ones, a slight improvement is better than none!
Thus, inhaling botanical essential oils might offer a noninvasive method for addressing cognitive decline and dementia.
Here is a list of essential oils that can boost the brain’s cognitive functions and soothe the nervous system:
Rosemary
“There’s rosemary, that’s for remembrance.” –William Shakespeare, Hamlet, 1601
Researchers have studied the impact of rosemary (Rosmarinus officinalis) essential oil on human short-term image and numerical memory. They found that aromatherapy was an efficacious non-pharmacological therapy for dementia.
Known for its memory-enhancing properties, rosemary essential oil can enhance mental clarity and alertness. Scientists are currently evaluating rosemary’s ability to delay Alzheimer’s progression.
Inhaling its invigorating scent before a vital task can make a significant difference. Research indicates that rosemary oil can help prevent the breakdown of a brain chemical called acetylcholine—a chemical messenger or neurotransmitter that plays a vital role in the brain and is linked to learning, concentration, and memory.
Smelling rosemary oil may have beneficial effects on:
- Cognitive function
- Functional performance
- Behavior
- Quality of life
- Relaxation
- Wandering
- Sleep
- Mood
Peppermint
 Peppermint (Mentha piperita) essential oil’s refreshing scent comes from its menthol content, making it a powerful tool for enhancing focus, concentration, and alertness by clearing mental fog.
Peppermint (Mentha piperita) essential oil’s refreshing scent comes from its menthol content, making it a powerful tool for enhancing focus, concentration, and alertness by clearing mental fog.
The scent of peppermint improves cognitive performance by stimulating the hippocampus, a part of the limbic system responsible for forming new memories, engaging emotions, and enhancing learning capabilities.
In one study, participants who inhaled peppermint oil saw a 28% improvement in their performance on a task that required attention and memory. Another study found that peppermint oil sniffing therapy improved cognitive function in patients with mild cognitive impairment. A pilot study also found that peppermint aroma positively affected cognitive function and psychomotor skills in patients with dementia.
Besides supporting memory in Alzheimer’s patients, peppermint oil has been found to stimulate appetite, reduce anxiety, and relieve headaches.
 Lavender
Lavender
While often associated with relaxation, lavender (Lavandula angustifolia) essential oil reduces stress and anxiety, promoting a calm state of mind conducive to clear thinking.
Lemon
Lemon (Citrus limon) essential oil’s invigorating, bright, cheerful aroma can lift the spirit, increase energy levels, and improve mental alertness. It stimulates the central nervous system, positively affecting cognitive functioning, attention levels, memory, and mood
Research suggests that lemon essential oil can regulate synaptic plasticity and hippocampal-dependent memory function and provide protection against Alzheimer’s disease-related synaptic loss and memory impairment.
Basil
Basil (Ocimum basilicum) essential oil, used in Ayurveda, can significantly reduce confusion and forgetfulness, stimulating the prefrontal cortex. It enhances mental clarity by stimulating the prefrontal cortex.
Its active compounds, such as linalool and eugenol, have been found to increase cerebral blood flow, clearing mental fog. The results are improved focus, attention, and mental performance. Reduced stress leads to a relaxed mind and body, promoting overall wellbeing
Melissa
Melissa (Melissa officinalis), also known as Lemon Balm, melissa is one of the most studied essential oils for its effect on people with Alzheimer’s disease. It is known for its calming effect, easing anxiety, stress, and nervous conditions related to agitation in dementia. The University of Melbourne found that inhaling lemon balm boosted cognition and alleviated anxiety and depression.
Cypress
 Cypress (Cupressus sempervirens) oil provides system-wide neurological support. Its sedative effects induce a calm in the central nervous system, promoting a relaxed feeling of emotional stability, comfort, and support. It enhances memory recall, boosts focus and concentration, and aids in balancing moods.
Cypress (Cupressus sempervirens) oil provides system-wide neurological support. Its sedative effects induce a calm in the central nervous system, promoting a relaxed feeling of emotional stability, comfort, and support. It enhances memory recall, boosts focus and concentration, and aids in balancing moods.
It is also energizing and stimulates feelings of happiness and ease. This can be particularly helpful for people who are undergoing emotional stress, have trouble sleeping, or have experienced recent trauma or shock.
Furthermore, cypress essential oil is antispasmodic and antibacterial. It supports lung function by clearing congestion and eliminating phlegm.
Fir
Fir (Abies alba) essential oil is another lesser-known but no less helpful oil for boosting memory and concentration. This scent soothes tension and reduces stress and anxiety in dementia patients while improving mental clarity, focus, and memory recall.
Vetiver
Inhaling vetiver (Chrysopogon zizanioides) essential oil may improve alertness and brain function by providing relaxing, soothing, and calming benefits. A well-known sedative, vetiver reduces emotional outbursts such as anger, anxiety, hysteric attacks, restlessness, and nervousness. It improves concentration and focus, relieving brain fog.
Clarity & Focus Spray
 Inhaling essential oils synergistically combined in our Alchemical Wellness formulas offers quick brain benefits, easing cognitive symptoms due to dementia.
Inhaling essential oils synergistically combined in our Alchemical Wellness formulas offers quick brain benefits, easing cognitive symptoms due to dementia.
Formulated to boost cognitive function and aid memory retention, Clarity & Focus Spray may enhance mental processing, attention span, focus, concentration, and memory while calming nerves and uplifting the mood.
The refreshing blend stimulates the part of the limbic system that controls memory, learning, and alertness, indirectly impacting focus and concentration by reducing stress levels.
Our aromatic synergy blend of organic essential oils includes lemon, basil, coriander, rosemary, cypress, fir, peppermint, melissa, and vetiver. Easy to use, simply mist around the head and body.
Memory Care
While there is no cure for Alzheimer’s disease or for most other causes of dementia at present, the problems associated with dementia, such as restlessness, depression, and anxiety, can be soothed with botanical scents. It may also be possible, especially in the early stages of dementia, to improve someone’s memory with aromatherapy.
Aromatherapy has become increasingly popular as a supplemental and non-pharmacological treatment for dementia and Alzheimer’s. Memory care communities can benefit from using Fleur’s Comfort Care Sprays and Oils and incorporating them into patients’ daily routines.
Using essential oils and understanding scent and memory can improve cognitive clarity, focus, and emotional wellbeing.
It is also possible to help people with dementia and their carers in various practical ways. These include ways of caring kindness for people with dementia that build on those affected’s strengths and abilities. This ensures that people with dementia maintain a sense of wellbeing and individuality throughout their illness.
Training for care professionals is crucial to effectively integrate complementary aromatherapy in treating and managing various health issues. A few of Fleur’s best customers are those caregivers who work to alleviate suffering in assisted living, memory, and hospice care settings.
Loving a Person with Dementia
“The problem is not that people with dementia forget. The problem is that they are forgotten. –John Swinton

Dementia is a general term for a group of neurological conditions that affect the brain and worsen over time, causing the loss of cognitive functioning.
Offering flower essence aromatherapy assistance, hope, and inspiration to individuals living with dementia and their caregivers is an opportunity to show love.
I opened my heart to my mother’s condition, allowing me to release my judgments of past hurts or future expectations. She responded to my kindness and displayed a child-like sweetness I had long experienced since childhood.
Recognizing the humanity in others provides valuable insight and understanding. Caring for someone with dementia requires approaching the situation with unwavering love, kindness, patience, and compassion.
 The brain-boosting synergy of essential oils in Fleur’s Comfort Care Memory Kit may stimulate the brain’s memory centers and stabilize your loved one’s decline.
The brain-boosting synergy of essential oils in Fleur’s Comfort Care Memory Kit may stimulate the brain’s memory centers and stabilize your loved one’s decline.
Our Memory Kit contains Clarity & Focus Spray, Amore Love Oil, and Stability Ritual Essence to ease symptoms related to age-related dementia that affect memory, cognitive impairment, and mood.
Summary
To summarize, essential oils’ remarkable benefits in enhancing brain function can significantly improve the condition of dementia patients, especially during early onset.
They also improve overall quality of life by uplifting mood, relieving depression, easing anxiety, reducing restlessness and agitation, and improving sleep.
I expect these insights will advance our understanding of learning and memory and have implications for addressing memory-related disorders.
All my aromatic love,
Vidya