The autonomic nervous system is the heart of our lived experience. –Deb Dana
As the seasons change, so does our aromatherapy focus this month. With the days becoming longer, we can look forward to celebrating the Summer Solstice later in the month on June 21.
In the meantime, in this blog, I’ll continue my discussion from my previous blog: Aromatherapy Mental Health. In that blog, I shared that we are biologically hard-wired to smell through the process of olfaction and how scent, memory, and emotion are intertwined.
We can learn to harness our sense of smell as an aromatherapy tool for supporting resiliency and healing from trauma as an integrative mental health treatment option.
Soothing an overactive brain and nervous system due to trauma’s emotional fallout and effects is possible. Since the autonomic nervous system is the heart of our lived experience, we can bring calm by increasing brain plasticity and rewiring the trauma pathways using the power of smell.
June is Post Traumatic Stress Disorder Awareness Month
There are currently about 8 million people in the United States with PTSD.
Now, more than ever, it is critical to be aware of the multifaceted effects of trauma on ourselves, our families, and our communities.
Post Traumatic Stress Disorder (PTSD) is a serious mental health issue. It’s estimated that around 3 in every 100 adults will experience it at some time, profoundly affecting their everyday existence.
People exposed to severe traumatic events (such as combat exposure) are clearly at risk for PTSD. Persistent or chronic PTSD can have a tremendous negative effect on a person’s daily life as well as physical and mental health.
My Family’s Story
 I don’t know anyone who PTSD hasn’t touched, my family included. When my father returned from serving in the Korean War, there was a lot of secrecy about his mental health. Unfortunately, his PTSD was never disclosed before he married and had children.
I don’t know anyone who PTSD hasn’t touched, my family included. When my father returned from serving in the Korean War, there was a lot of secrecy about his mental health. Unfortunately, his PTSD was never disclosed before he married and had children.
My father was physically abusive to our mother, the cat, and the dog. As a child experiencing his outbursts and his unconcern for his brutality, my mother, sisters, and I feared him.
His behavior sent shock waves through the family, leading him (and my mother) to use alcohol and pills to manage his mental-emotional pain. Sadly, my father’s psychological distress and anger were never professionally addressed before my parents were divorced.
My former husband and brother-in-law were both Vietnam veterans. Each experienced the war in their own way, but what they did share in common was the toll it took on their lives and the lives of their families.
My brother-in-law, who was in special forces, especially suffered from the long-term effects of PTSD. He became a victim of substance abuse impacting his family’s welfare in his attempt to manage his nightmares, startle reflexes, flashbacks, disassociation, and chronic physical pain. Even with help from Veterans Affairs, he struggled with depression and anxiety.
Alcohol abuse, addiction, depression, musculoskeletal pain, and other illnesses are frequently linked with PTSD and can cause problems in family and work life, creating further distress for veterans and those who care most about them.
My son-in-law was profoundly changed after his return from active duty in Afghanistan. He now avoids loud environments and isolates himself in a dark room at home to regain his composure. Fortunately, he’s gotten the help he needs to manage his mental health and his PTSD.
All these men struggled to understand the changes in their personalities and PTSD triggers through the years. They did their best to reintegrate back into their families and society. For the most part, through the years, with the help of psychotherapy (and some medication), they eventually became functioning, beloved members of their families.
Many of my younger clients suffer from some form of trauma due to growing up in families that never addressed unresolved parental stress. Some are traumatized by disparaging societal attitudes, bullying, and the pressure of an increasingly unsafe and uncertain world.
By raising awareness about PTSD, we can help reduce the stigma associated and help ensure that those suffering from the invisible wounds of trauma receive integrative treatment.
What is Trauma?
Trauma is a state of high arousal in which normal coping mechanisms are overwhelmed in response to the perception of threat. –Stephen Fortis
Trauma can be defined as any unresolved autonomic nervous system response. It’s about the nervous system’s reaction to an event, not necessarily the event itself—either experiencing or witnessing it. No one person reacts the same way. Even minor stress can trigger an out-of-proportion response.
 Trauma may be acute, chronic, or complex. There is intergenerational trauma, which happens through generations like the family lineage, where something traumatic happened somewhere in the family’s history. All types of trauma are important for us to understand.
Trauma may be acute, chronic, or complex. There is intergenerational trauma, which happens through generations like the family lineage, where something traumatic happened somewhere in the family’s history. All types of trauma are important for us to understand.
When looking at trauma, it is important to assess it on a deeper cellular level. The visible signs are only a part of the trauma that affects the body. Trauma affects us to the deepest part of our being. It can rewire our thoughts, actions, and reactions, changing our genes and DNA’s structure and programming.
Consequently, trauma can leave a chemical mark on a person’s genes, causing epigenetic markings. This happens due to an increased acidity in the body. These markings are well known to be passed down generationally.
Epigenetic changes are reversible and do not change your DNA sequence but can change how your body reads a DNA sequence.
Trauma & The Brain
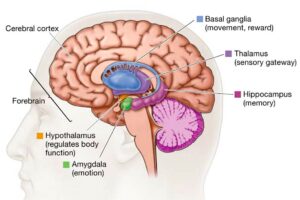 Trauma can affect the function of the brain and how parts of the brain connect. It profoundly affects the brain, specifically the emotional part of the brain, the amygdala, the hippocampus, and the prefrontal cortex.
Trauma can affect the function of the brain and how parts of the brain connect. It profoundly affects the brain, specifically the emotional part of the brain, the amygdala, the hippocampus, and the prefrontal cortex.
Our brain (the amygdala) has an evolutionary basis for protecting us from danger. Traum causes the brain to “misfire” because it cannot distinguish between life-threatening and non-life-threatening stressors.
It’s like a false alarm that is constantly going off. Our amygdala gets stuck in “on” mode, affecting the nervous system. So we run away from or fight danger all day long and at night too!
When the emotional part of the brain is overactive due to constantly being in survival mode, the memory part of the brain, the hippocampus, is continuously activated, which means the person is always running on adrenaline.
Adrenaline is also known as the fight-or-flight hormone. It is released in response to a stressful, exciting, dangerous, or threatening situation so that we can take action.
Chronic stress is found to cause profound, long-lasting physical changes in the brain. It activates and exacerbates inflammation in the peripheral immune system due to an overabundance of cortisol in the body.
The good news is the brain can reorganize itself and change its structure and function using thought patterns. The brain is neuroplastic, meaning the neurons can change their structure and function in response to internal or external stimuli.
What is PTSD?
Post Traumatic Stress Disorder (PTSD) is, by its name, a stress disorder described as the ‘aftermath of shock.’ PTSD includes a cluster of body-mind symptoms that persist after a person has survived a traumatic event.
Some people develop PTSD after exposure to extremely traumatic events. Traumatic events fall anywhere on a continuum from combat due to war, or terrorist attacks, to victims of crime, gun violence, childhood abandonment, physical, sexual, or emotional abuse, accident, or natural disaster.
We might think only combat veterans experience PTSD, but this condition doesn’t discriminate. People can also have PTSD from having a life-threatening medical condition or undergoing invasive surgery.
PTSD may develop differently among occupational, gender, and age groups. Women are about twice as likely as men to develop PTSD.
Children are vulnerable to developing PTSD after exposure to a traumatic event, though the symptoms may differ for young children, older children, adolescents, and adults. Just ask the kids exposed to gun violence in their schools and communities.
PTSD Risk
The impact of PTSD is not limited to those diagnosed with the disorder. Anyone who lives with or cares for PTSD patients is also affected. PTSD risk also is increased by the cumulative effect of multiple, severe, uncontrollable traumas and personal factors such as:
- History of childhood abuse or disruption in attachment
- Personal or family history of psychiatric illness
- Limited social support
- Passive coping mechanisms
- Neurotic or introverted personality style.
Considering this, the consequences of PTSD are staggering.
Physiological Symptoms
Extreme stress and fear reactions are a natural nervous system response to danger and threat. When triggered, people with PTSD experience involuntary physical fight-flight symptoms such as
- Breathing becomes quicker and more shallow
- Increased blood pressure and elevated heart rate
- Dry mouth
- Changes in vision
- Muscle tension
- Cold hand – sweaty palms
- Bladder urgency.
The effect of traumatic exposure over time not addressed may trigger a range of chronic health conditions, including but not limited to
- Severe headaches
- Fibromyalgia
- Heart disease
- High blood pressure
- Asthma
- Arthritis
- Peptic ulcers
- Chronic lung disease
- Stroke
- Joint, back, or other types of pain
- Disturbed sleep
- Exaggerated startle response
- Hypervigilance.
Psychological & Emotional Symptoms
The far-reaching effects of PTSD are distinguished by psychological and emotional pain. Traumatic events can feel so life-threatening that they completely change how our minds react to every experience.
Besides stress, PTSD is characterized by anxiety. The amygdala is our body’s anxiety switch. This part of the brain has much to do with physiological responses to stressors.
Anxiety and panic attacks can be triggered differently for each of us, but they usually produce the same response in everyone — overwhelming waves of emotion.
The stress reaction to a traumatic event shuts down episodic memory. It leads to a series of negative emotional loops that have an even more significant adverse effect on the brain.
About 80% of people living with PTSD are diagnosed with anxiety, dissociation, mood (irritation, anger, and depression), or somatoform disorders (a mental health condition that causes an individual to experience physical bodily symptoms in response to psychological distress) with delayed reactions, personality disorders, and substance abuse disorder.
PTSD psychological and emotional symptoms are generally grouped into four types:
- Intrusive memories
- Avoidance
- Negative changes in thinking and mood
- Changes in physical and emotional reactions.
Symptoms can vary over time or vary from person to person. But for the most part, people with PTSD may relive the trauma in painful recollections, flashbacks, or recurrent dreams or nightmares.
For some people, emotions may become volatile. Overreacting to simple situations can lead to feelings of overwhelm and loss of control.
Signs of Emotional Trauma:
- Anxiety, worry, intense fear
- Shock, denial, or disbelief
- Anger, irritability, mood swings
- Feeling sad or hopeless about the future
- Feeling disconnected from what’s around you or feeling numb
- Confusion
- Difficulty concentrating or remembering
- Guilt, shame, self-blame
- Withdrawal from what previously provided pleasure.
Acute emotional hair-trigger reactions can set off physical stress reactions, including panic attacks or a racing heart.
Trauma-Related Dissociation
Some of my clients with a history of trauma experience body sensations that they do not fully understand. Subsequently, they experience them as aversive.
As a survival mechanism, Trauma-Related Dissociation is sometimes described as a ‘mental escape’ when physical escape is not possible or when a person is so emotionally overwhelmed that they cannot cope any longer.
Because symptoms feel outside the survivor’s control, they can cause fear, confusion, and cognitive dissonance. People with dissociation may often be misdiagnosed and have a lot of medical treatment that does not help them.
Although these reactions are usually temporary, dissociation may last longer in severe or repeated trauma cases. This can be frightening and difficult to explain to others.
Thus, it is common for trauma survivors to experience automatic body reactions to which they make attributions concerning responsibility and blame, with an expected result being an experience of shame.
The complexity of the multifaceted symptoms of PTSD can be a crucial barrier for those assessing and seeking treatment.
PTSD and Disrupted Relationships
PTSD directly impacts relationships and is associated with subsequent decreases in positive social support and an increase in highly conflictual interpersonal relations. Disconnection from important social relations may lead a person to feel misunderstood, alone, and adrift, affecting everyone.
Negative thought pattern loops contribute to how they feel about themselves, their self-image, and how they navigate the world. It is challenging to connect to others if you cannot connect to yourself and identify what you’re feeling. People with PTSD frequently struggle with low self-esteem and self-worth.
Intense emotional reactions to remembering trauma cause a tendency toward isolation and avoidance of activities, places, and sometimes people who may trigger the memory of the traumatic event.
Those living with PTSD can be in a state of constant fear and no longer aware of potentially threatening or harmful scenarios. Intimate partner violence impacts children who witness their parents fighting, putting them at greater risk.
Even when they have worked hard to heal, they are sometimes vulnerable to being triggered by an event that unearths those painful moments.
Rewiring the Traumatic Brain
As we delve into the complex relationships among our brains, minds, and social interactions, we can better comprehend the root causes of our clients’ struggles, ultimately leading to more effective therapeutic interventions.
It might seem like trauma does irreversible damage to the brain, but that’s not true. Our brains are highly adaptable. Neuroplasticity, the brain’s ability to form new connections, explains why we can rewire our brains to reverse trauma’s damaging effects.
Neuroplasticity can be defined as the ability of the brain to change its structure and function in response to an input.
Many people have benefited from rehabilitation programs aimed at treating PTSD. While research is ongoing, the current body of knowledge on neuroplasticity is already shaping therapeutic practices and is a vital concept to understand in brain rehabilitation.
It is scientifically proven that replacing harmful and destructive thoughts with positive and uplifting thoughts will rebuild and restructure the pathways in the brain.
The olfactory network in our brains is particularly neuroplastic.
When we frequently use the many parts of the brain involved in smelling through repeated exposure to aromas from essential oils, it’s possible to rewire the brain’s traumatic pathways through the nose.
The Blood-Brain Barrier
Essential oils have proven medicinal properties and can amplify the effectiveness of treatment for PTSD. Research with essential oils offers a nonpharmaceutical option due to their ability to cross the blood-brain barrier.
One of the gateways botanical essential oils use to enter the body is via the respiratory system. Inhaling a botanical aroma is one of the most effective ways to use oil because of its quick absorption. Thus, when we smell specific aromas, their molecules will pass through the blood-brain barrier affecting the brain and the nervous system.
Evidence shows that essential oil chemical constituents assist with neurological health by increasing oxygen transport to the limbic system and increasing the secretion of endorphins, neurotransmitters, and antibodies.
In the case of trauma, the brain (amygdala) interprets the aroma to release the trauma bonds locked up in the amygdala and the limbic system. Since the brain processes odors in the same localities as memory, cognition, and mood, essential oils can be master teachers and psychological healers.
Today we can learn how to heal from PTSD with support from flower essences and aromatherapy.
PTSD Relief with Botanical Aromatherapy
PTSD may be treated with aromatherapy through the same mechanisms I discussed in my previous blog: Aromatherapy Mental Health.
Aromatherapy utilizing botanical essential oils is a practical and valuable tool for treating sufferers of PTSD and their families. I’ve used potent blends of essential oils as therapeutic allies when working with clients to help reduce symptoms of PTSD, especially anxiety, depression, and insomnia, improving physical and mental well-being.
The best essential oils are calming, grounding, and comforting, evoking embodied feelings of safety and security.
Fleur Flower Essence Aromatherapy
Many Fleur comfort care products are formulated to help the automatic nervous system safely calm down.
Our alchemical wellness care blends to assist with emotional healing and processing trauma. They aid in decoding body trauma memories and trauma frequencies and blocked emotions connected to them.
The following alchemical wellness care blends are recommended when working with anyone who has PTSD:
- Anxiety Relief Spray
- Anxiety Relief Tincture
- Deha Muscle Soothe Oil
- Nidra Rest & Restore Oil
- Prasanta Calming Oil
- Shanti Serenity Oil
- Magnesium Lotion
Their therapeutic benefits help properly manage anxiety, insomnia, and depression through various implementation methods, such as inhalation, massage, and trigger point therapy.
Anxiety Relief Spray
Looking for a solution to manage PTSD? Try our Anxiety Relief Spray. It might just be the answer when PTSD stress and anxiety become unmanageable.
 Anxiety Relief Spray is formulated with organic essential oils of Sweet Orange, Rose Geranium, and Ylang Ylang. Their synergy helps interrupt the traumatic pathways that lead to anxiety and panic attacks due to the flight-fight sympathetic nervous system.
Anxiety Relief Spray is formulated with organic essential oils of Sweet Orange, Rose Geranium, and Ylang Ylang. Their synergy helps interrupt the traumatic pathways that lead to anxiety and panic attacks due to the flight-fight sympathetic nervous system.
When misted about the head and body, breathing deeply, the aroma quickly soothes the symptoms of an overactive nervous system allowing the person to calm down and feel more resourced. Anxiety Relief Spray is safe to use for anyone of all ages.
One client of mine who suffers from childhood PTSD uses Anxiety Relief Spray when she notices physiological arousal leading to emotional flooding, anxiety, and panic attack. She says:
“This Spray helps me calm myself. I love how it smells. When I feel a panic attack coming on, after spraying myself, I can breathe again so I can use my self-talk tools. I stop spiraling into a deep well so that I don’t become overwhelmed with fear. I’ve also noticed since using the Spray that my anxiety is less, and my mood swings are less intense.”
Nidra Rest & Restore Oil
Nidra Rest & Restore Oil is alchemically formulated to help the overactive sympathetic nervous system let down so that repair at the cellular level may take place.
PTSD and sleep have a complex relationship. Though sleep problems accompany many mental health conditions, sleep problems in PTSD are considered part of the disorder.
Long-lasting sleep disturbances are a core feature of PTSD. Among the symptoms used to diagnose PTSD, two are directly related to sleep: hyperarousal and intrusion, which can manifest as insomnia and nightmares.
The earthy aroma of organic soporific essential oils of Spikenard, Vetiver, Neroli, Valerian, Hops, Clary Sage, Roman Chamomile, Celery, Ylang Ylang, and Patchouli encourages deep brain and nervous system repair while you sleep when your subconscious mind defragments and processes daily stressors and stored trauma.
Rub a small amount into your hands and the soles of your feet before bed to benefit your sleeping well.
Another client who has suffered from insomnia for years said this after he used Nidra Rest & Repair Oil:
“Your Nidra oil is miraculous. That was truly the best sleep I’ve had in a very long time. I had beautiful, rich dreams, and I woke without feeling groggy. Thank you so much for the blessing of this healing substance.”
A Few Essential Oil Helpers
Ylang Ylang Essential Oil
 The sweet smell of Ylang Ylang essential oil is steam distilled from the Cananaga odorata flowers.
The sweet smell of Ylang Ylang essential oil is steam distilled from the Cananaga odorata flowers.
This oil is excellent for easing PTSD symptoms, and reducing tension, stress, and anxiety, primarily associated with heart palpitations and other nervous system-related conditions.
Several clinical studies have shown that the aroma of Ylang Ylang is ideal to use during times of shock and trauma, especially during panic attacks.
When inhaled, this aroma significantly reduces blood pressure and heart rate, which lowers stress responses and reduces anxiety. It assists with relaxation, improving mood, and dispelling negative emotions.
Ylang Ylang is a beautiful nervous system soother known for its mild sedative effects and stabilizing emotions. I’ve used this essential oil in blends for Anxiety Relief Spray and Nidra Rest & Restore Oil.
Rose Geranium
 Rose Geranium essential oil is steam distilled from the leaves of the Pelargonium graveolens shrub.
Rose Geranium essential oil is steam distilled from the leaves of the Pelargonium graveolens shrub.
In cases of recovery from PTSD, Geranium oil’s warm, rosy smell helps the brain process anxiety, grief, and intense stress. Emotionally, it targets trauma bonds located in the amygdala, relieving overwhelming crying and easing mood swings.
It uplifts, energizes, and benefits mental health by dispelling depression, reducing irritation and anger, and managing overpowering emotions and those struggling to express them.
It is a beautiful aroma for people deeply hurt from past traumas, trapped in large heart wounds from loss, sexual abuse, and or abandonment. Rose Geranium’s aromatic gift helps create a nurturing sense of security and stability while dissolving tension and anxiety.
Flower Essence Vibrational Support
Our Alchemical Wellness Sprays and Oils contain wildflower essences from the outback. They enhance the healing properties of our formulas and work in synergy with essential oils to rebalance and align a shattered subtle body.
Flower essence and vibrational essences work with the fragmented self to empower clients to re-discover their own spiritual resources for healing soul wounds during their recovery journey. They help transform negative emotions and thought patterns to help the person reclaim themselves and move forward in life.
The following stand-alone vibrational essences are beneficial when recruiting an integrative approach to healing the spirit during recovery. Energetically they are powerful allies for supporting mental, emotional, and spiritual wellness.
Unlike our Sprays and Oils, these remedies are meant to be taken internally. Simply add 2-3 drops to your drinking water, or apply to the top of your head or under your tongue to experience rapid calming relief, emotional fortitude, and feel safe again.
They can be safely used alongside other forms of therapy or with medication. They are an excellent choice when using aromatherapy isn’t convenient or practical.
 Anxiety Relief Vibrational Remedy
Anxiety Relief Vibrational Remedy
Anxiety Relief Tincture was created with the same wildflower and vibrational essences I use in our Anxiety Relief Spray.
This vibrational remedy is ideal for people with PTSD and who struggle with ongoing anxiety. It will help calm escalating panic on the verge of a breakdown and feelings of fear of losing control of their mind bringing relief to the body-mind.
Resilience Ritual Essence
Resilience Ritual Essence captures the resilient essence of the Arbutus Tree. It is a beautiful essence to help fortify the mind and spirit after shock and trauma. It is especially helpful for working with enduring challenging PTSD conditions to impart the courage to work with therapeutic protocols that restore healthy mind-body-spirit functioning.
Stability Ritual Essence
Stability Ritual Essence captures the long-standing stability of the Redwood Tree. This essence is helpful when you need the strength to take a stand, firmness to resist the wild up and down quakes of fear, anxiety, overwhelming emotional flooding, or dealing with recurring intense feelings of pain, sadness, or grief. This essence increases stable equilibrium and aids with maintaining perspective in the here and now.
Refuge Ritual Essence
Feeling safe and secure after experiencing trauma may seem daunting to a survivor. Refuge Ritual Essence can help with finding sanctuary within. This vibrational essence captures the spirit of hope (and forgiveness) for restoring the belief in a second chance for a life well lived.
Refuge Ritual Essence helps the person meet adversity by transforming fear, converting the paralysis of anxiety into feeling safe in the world again. This remedy connects one’s inner sources of emotional and spiritual strength and courage with forgiveness, compassion, and gratitude.
PTSD Recovery
Trauma recovery is possible. PTSD recovery is a gradual, ongoing process. It doesn’t happen overnight, nor does the consequences of trauma ever disappear completely. This can make life seem difficult at times.
Sometimes people are reluctant to seek help for PTSD because they want to handle it themselves. Hiding pain is a consequence of shame. A traumatizing experience complicated by PTSD can leave a person feeling stuck.
Rather than allowing the trauma to be in control, it is important to remember that there is no stigma for reaching out and asking for the help you deserve. Getting treatment for PTSD can help you to fight back and regain your sense of control over the powerful hold of trauma.
Recovering from PTSD involves helping the nervous system return to its pre-trauma state of balance. While this process is easier with the guidance and support of an experienced therapist, you don’t need to wait for a medical appointment to start feeling better.
We owe it to ourselves and our families to share our empathy and compassion for the suffering that PTSD imparts and the toll it takes on our lives. Including the healing support of natural remedies such as flower essence aromatherapy is immensely helpful in reestablishing a sense of connectivity and wholeness.
In my counseling practice, clients who have experienced trauma work hard to feel safe enough and calm enough each day. I help them learn to shape their automatic responses through polyvagal, cognitive behavioral interventions and mindfulness-based practices.
I encourage aromatic protocols and lifestyle strategies that complement the clients’ capacity to become resilient and successfully cope with PTSD symptoms and regain control of their lives. Many eventually wean themselves off their antidepressants and antianxiety meds.
For a Better Life
In this blog, I shared how trauma affects the nervous system and brain. I outlined what trauma is and how PTSD is a serious mental health issue.
Through PTSD awareness, we can begin working with trauma by understanding how the brain processes sensory inputs through the olfactory system.
Soothing an overactive brain and nervous system due to trauma’s emotional fallout and effects is possible. Since the autonomic nervous system is the heart of our lived experience, we can bring calm by increasing brain plasticity and rewiring the trauma pathways using the power of smell.
Regaining a feeling of safety and security by treating trauma using an integrative body-mind approach, aromatherapy, and vibrational essences can provide us with better ways to manage PTSD symptoms for a better life.
All my aromatic Love,
Vidya



